7 Ways to Properly Design a Modern Medical Office Interior — Patient‑Centered, Efficient & Compliant
Designing a medical office isn’t just about picking pretty tiles or a nice logo. A well‑designed medical interior improves patient comfort, increases staff efficiency, lowers infection risks, and helps meet legal accessibility and occupational-safety requirements. This guide walks you through 7 proven ways to design a modern medical office interior that balances function, safety, and a calm patient experience.
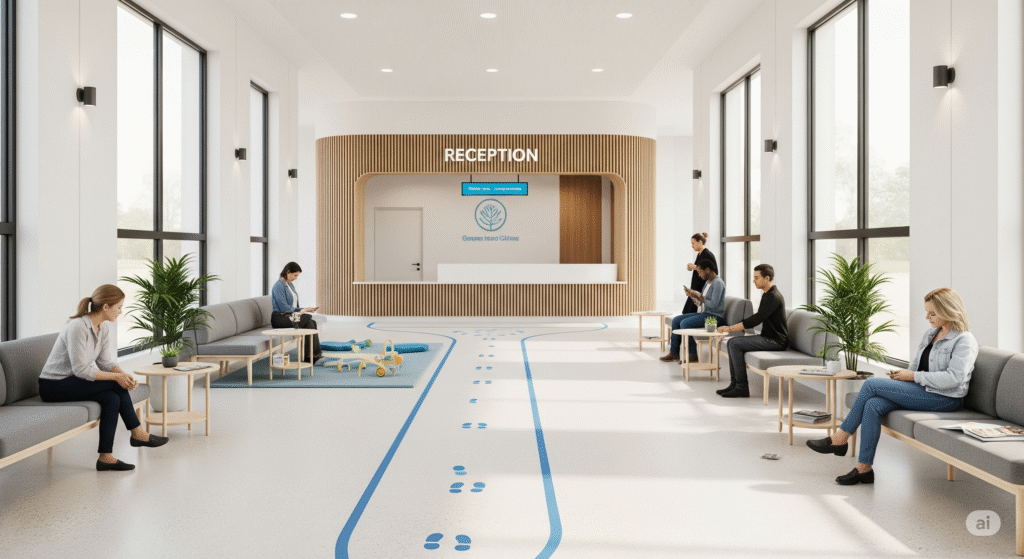
1. Prioritize patient flow and smart zoning
A clear, logical flow reduces confusion, waiting times, and accidental cross-traffic between clinical and non-clinical zones.
Practical steps:
- Map patient arrival to departure: entrance → reception → waiting → triage/exam → checkout → exit.
- Create separate staff-only corridors and clinical support zones (labs, supply closets) to keep patients out of staff work areas.
- Use visual cues (floor finishes, subtle color changes, signage) to indicate transitions between areas.
- Design waiting areas so arrivals don’t bottleneck at reception — consider a recessed reception desk or side check-in kiosks.
Why it matters: Efficient flow reduces staff steps per patient, speeds appointments, and improves safety by isolating clinical traffic.
2. Design for infection control and durable materials
In medical settings, materials and finishes must be cleanable, durable, and non-porous to support infection-control protocols.
Material recommendations:
- Floors: sheet vinyl or seamless resilient flooring for easy cleaning.
- Walls: semi‑gloss or washable paint; high‑impact wall protection in corridors.
- Countertops: solid-surface (e.g., quartz) or other non-porous materials.
- Upholstery: vinyl or performance fabrics with antimicrobial finishes.
Layout considerations:
- Hands‑free fixtures (faucets, soap dispensers, door openers) where possible.
- Easily accessible hand hygiene stations near exam rooms and entrances.
- Design exam rooms to allow for efficient cleaning (minimal clutter, wall-mounted equipment where feasible).
Why it matters: Proper materials reduce infection risks and lower maintenance costs.
3. Optimize lighting for comfort and clinical needs
Lighting affects both clinical performance and patient comfort. A layered lighting approach reduces glare and supports accurate diagnosis.

Lighting strategy:
- Ambient lighting: soft, even general illumination for waiting and corridors.
- Task lighting: bright, adjustable lights over exam tables and workstations.
- Accent lighting: to highlight wayfinding, art, or feature walls.
- Use dimmable fixtures in consultation rooms or procedure rooms to adapt to different tasks.
Technical tips:
- Aim for neutral color temperatures (3500K–4000K) in clinical areas; warmer tones (2700K–3000K) in waiting rooms for a calming effect.
- Ensure CRI (Color Rendering Index) is high (90+) where color accuracy matters (e.g., dermatology labs).
Why it matters: Proper lighting reduces clinician fatigue, improves diagnostic accuracy, and enhances patient wellbeing.
4. Accessibility & ADA compliance — make access universal
Accessibility isn’t optional. Follow ADA guidelines (or your country’s equivalent) to ensure the office is usable by people of all abilities.
Accessibility checklist:
- Door widths, ramp slopes, and clear turning radii for wheelchairs.
- Accessible washrooms, grab bars, and appropriately mounted sinks.
- Clear, high-contrast signage and tactile elements where needed.
- Reception counters with a lowered section for wheelchair users and clear sightlines for hearing‑impaired visitors.
Design tip: Consult a local accessibility specialist early—compliance is easier and cheaper when integrated at design stage.
Why it matters: Accessibility improves patient access, reduces legal risk, and enhances reputation.
5. Integrate technology thoughtfully (without overwhelming the space)
Modern clinics need reliable IT — EHR stations, Wi‑Fi, telehealth setups, and medical device connectivity — but technology should support care, not dominate the room.
Integration tips:
- Provide a dedicated workstation in each exam room with ergonomic chair and cable management.
- Conceal wiring and equipment behind panels or in recessed cabinetry to maintain a calm environment.
- Plan for future tech: include extra data conduits, power drops, and flexible wall space for monitors.
- Use wall-mounted tablets or kiosks for patient check-in where appropriate, but keep a staffed option for patients who prefer in-person help.
Data & privacy: Ensure server rooms and network equipment are secure and ventilated. Place screens so PHI (Protected Health Information) isn’t visible to other patients.
Why it matters: Thoughtful tech boosts staff efficiency and patient satisfaction while protecting sensitive data.
6. Choose ergonomic, hygienic furniture and flexible layouts
Furniture should be comfortable, cleanable, and flexible to support changing needs (e.g., switching an office to a telehealth room).
Furniture guidelines:
- Invest in modular seating for waiting areas so pieces can be cleaned or rearranged easily.
- Use exam tables with removable covers or antimicrobial surfaces.
- Provide sit‑stand options for workstations to support staff health.
- Choose mobile carts for equipment so rooms can be reconfigured quickly.
Space planning: Design exam rooms that are slightly larger than minimum code where possible — this improves maneuverability for staff and equipment.
Why it matters: Ergonomic furniture reduces staff injuries and improves patient comfort.
7. Branding & calming aesthetics — design for trust and reduced anxiety

A medical office should communicate competence and care. Thoughtful aesthetics (colors, art, textures) help reduce patient anxiety and reinforce trust.
Aesthetic considerations:
- Choose a calm color palette — muted blues, greens, and warm neutrals often work well.
- Use nature imagery or biophilic elements (plants, natural textures) to improve mood.
- Display clear, professional signage and visible accreditation or provider credentials.
- Keep clutter out of sight: visible clutter increases patient stress and appears unprofessional.
Graphic wayfinding: Use consistent iconography and typography for easy navigation.
Why it matters: The right aesthetic supports the patient experience and strengthens your practice brand.
Why Layered Lighting in Your Kitchen Matters in 2025: A Complete Guide to Style & Function
Room-by-room quick checklist (printable)
Reception & waiting
- Recessed reception desk or side check-in.
- Seating modules with spacing for privacy and infection control.
- Clear signage and a low ADA counter.
- Hand sanitizer station near entrance.
Exam rooms
- Hands‑free sink, task lighting, durable surfaces.
- EHR workstation with cable management.
- Sufficient storage for supplies and mobile cart parking.
Procedure room / minor surgery
- Medical-grade finishes, scrub sink nearby, separated HVAC if required.
- Proper lighting levels and scrub storage.
Staff areas & back office
- Ergonomic desks, lockers, and a private break area.
- Secure storage for sensitive records and supplies.
Costs & phasing suggestions
Designing or renovating a medical office can be done in phases:
- Phase 1 — Essentials (0–6 months): Patient flow updates, reception remodel, signage, basic infection-control upgrades.
- Phase 2 — Clinical & tech upgrades (3–12 months): Exam room finishes, lighting, EHR workstations, network upgrades.
- Phase 3 — Branding & comfort (6–18 months): Furniture refresh, art, landscaping/biophilia, full signage.
Tip: Prioritize elements that affect safety and patient flow first. Cosmetic touches can come later but should follow a consistent palette and brand guide.
External resources & references (helpful, authoritative)
- Centers for Disease Control and Prevention (CDC) — infection control recommendations for healthcare facilities.
- Americans with Disabilities Act (ADA) — accessibility guidelines (or your country’s equivalent accessibility authority).
- Occupational Safety and Health Administration (OSHA) — workplace safety standards.
- American Institute of Architects (AIA) — resources on healthcare design best practices.
- Local health department — for licensing and building-code requirements.
(Include local/regional resources and consultants when planning — laws and codes vary by location.)
Frequently Asked Questions (FAQs)
Q1: How much space does a typical exam room need?
A: Minimum sizes vary by code and specialty, but a practical exam room is often 100–130 sq ft to allow equipment and staff movement. Always check your local building codes and consider slightly larger rooms for better accessibility.
Q2: What flooring is best for medical offices?
A: Seamless resilient flooring (sheet vinyl or homogeneous vinyl) and certain rubber floors are excellent for ease of cleaning, durability, and slip resistance.
Q3: How can I make a small clinic feel less cramped?
A: Use light, warm color palettes, glass partitions where privacy allows, recessed storage, and multi-purpose furniture. Good lighting and decluttered surfaces also help.
Q4: How do I balance tech needs and patient privacy?
A: Position monitors so screens aren’t visible to other patients, use privacy screens, design receptionist areas with privacy barriers, and use secure network practices for PHI.
Q5: Do I need a separate HVAC system for procedure rooms?
A: That depends on the type of procedures you perform and local regulations. More invasive or sterile procedures often require separate HVAC or specific ventilation standards—consult your local codes.
Q6: Can I renovate in phases without disrupting patients?
A: Yes — stagger construction during off-hours, close and renovate one area at a time, and use temporary partitions. Communicate clearly with patients about any changes.
Final thoughts & next steps
Designing a modern medical office requires balancing safety, efficiency, and patient comfort. Start with patient flow, choose infection-resistant materials, and integrate technology in ways that support care without overwhelming the space. If you’re unsure where to begin, consult a healthcare-savvy architect or an interior designer experienced in medical facilities — early planning saves money and reduces compliance headaches.
